The modern medical era began when an absent-minded British scientist named Alexander Fleming returned from vacation to find that one of the petri dishes he forgot to put away was covered in a bacteria-killing mold. He had discovered penicillin, the world’s first antibiotic.
Ninety years later, the world faces an antibiotic crisis. Superbugs have evolved resistance to dozens of drugs in doctors’ arsenals, leading to infections that are increasingly difficult to treat. Global deaths from antibiotic-resistant infections are predicted to hit 10 million a year by 2050. So in labs around the world, scientists are racing against time to cultivate new microbe-destroying molecules – but most of the low-hanging fruit has already been picked.
With due respect to Fleming, microbiologist Sean Brady thinks it’s time to shift tactics. Instead of growing antibiotics in a petri dish, he hopes to find them in the ground.
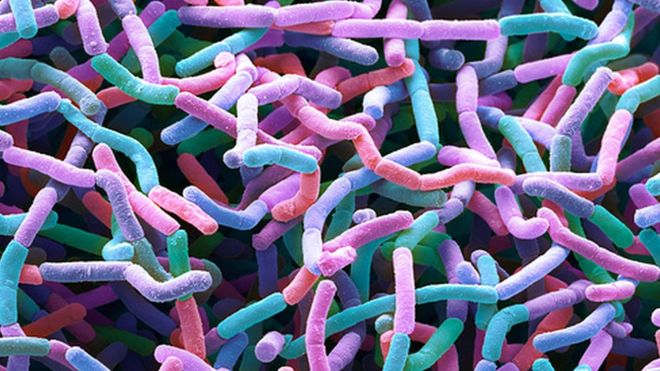
“Every place you step, there’s 10,000 bacteria, most of which we’ve never seen,” said Brady, a professor at Rockefeller University in New York. Many of these bacteria behave in ways that aren’t yet understood and produce molecules that haven’t been seen before.
“Our idea is, there’s this reservoir of antibiotics out in the environment we haven’t accessed yet,” Brady said.
That idea is beginning to pay off: In a study published Monday in the journal Nature Microbiology, he and his colleagues report the discovery of a new class of antibiotic extracted from unknown microorganisms living in soil. This class, which they call malacidins, kills several superbugs – including the dreaded methicillin-resistant Staphylococcus aureus (MRSA) – without engendering resistance.
You won’t find this antibiotic at your pharmacy next week, Brady cautioned. It takes years for a novel molecule to be developed, tested and approved for distribution. But its discovery is proof of a powerful principle, he said: A world of potentially useful untapped biodiversity is still waiting to be discovered.
Though antibiotics are prized for their ability to combat the microbes that make humans sick, most of them actually come from bacteria. For example, streptomycin, which has been used to treat tuberculosis and plague, is produced by the bacterium Streptomyces griseus. (This microbe was originally found in the dirt of a New Jersey farm field, though the antibiotic research was conducted using cell cultures.)
Bacteria have been fighting one another for billions of years – far, far longer than humans have been around – so it’s hardly surprising that they have evolved all the best weapons. Yet the vast majority of these microbes don’t grow well under controlled laboratory conditions, making them difficult to study.
“Maybe, using that simple culture-based approach, we’ve missed most of the chemistry that are produced by bacteria,” Brady said.
It would be better to derive interesting molecules directly from the environment. And with the advent of metagenomics, techniques that allow all the genetic material in a sample to be sequenced en masse, researchers can do just that.
For this study, Brady’s team cloned vast quantities of DNA from hundreds of soil samples contributed by citizen scientists across the country and then sorted through the material in search of interesting sequences.
“Most of what’s there is completely unknown, and that’s the future,” Brady said.
He and his colleagues were looking specifically for a known gene associated with the production of calcium-dependent antibiotics – molecules that attack bacterial cells, but only when calcium is around. It’s thought that the existence of such an “on-off” switch may make it harder for microbes to evolve resistance. Because of this, the gene for calcium dependence might serve as a flag for a much longer sequence controlling the production of antibiotics – much the same way that coming across instructions for making crust might flag cookbook readers that they’ve found a recipe for pie.
Having identified a sequence containing the calcium-dependence gene, the researchers cloned it and injected it into a microbe that can be cultured. Soon enough, those microbes were making malacidins. When applied to cuts in the skin of MRSA-infected rats, the previously unknown molecule successfully sterilized the wounds. The bacterium didn’t show signs of resistance, even after three weeks of exposure.
According to Brady, malacidins work by interfering with the process that bacteria use to build their cell walls. Human cells rely on a different process, so the antibiotic isn’t toxic in people.
He and his colleagues don’t know what species the molecules come from, but they don’t need to – they already have the genetic blueprint for building it. “The effort now is to scale it,” he said.
Two years ago, Brady launched a company called Lodo Therapeutics, which aims to accelerate the discovery process and ultimately produce new medications that can be used to treat disease.
Brady is not the only scientist with this idea. Researchers elsewhere are using metagenomics to seek out new antibiotics in ocean water and insect guts. Meanwhile, the same technique has been applied to urban sewage and polluted lakes to reveal the vast extent of antibiotic resistance.
Speaking to the Los Angeles Times, Northeastern University microbiologist Kim Lewis noted that searching for the calcium-dependence gene allowed Brady’s team to sort through massive amounts of DNA. “They’ve used a clever approach to mine for antibiotics,” he said.
But Lewis, who was not involved in the research, pointed out that Brady and his colleagues will need to continue identifying new DNA signatures associated with antibiotics for their technique to keep working: “Now we need to say, ‘You guys can do even better.’ ”