A team of researchers, led by Trisha L. Andrew, professor of chemistry and chemical engineering at the University of Massachusetts Amherst, recently announced that they have synthesized a new material that solves one of the most difficult problems in the quest to create wearable, unobtrusive sensitive sensors: the problem of pressure.
“Imagine comfortable clothing that would monitor your body’s movements and vital signs continuously, over long periods of time,” says Andrew. “Such clothing would give clinicians fine-grained details for remote detection of disease or physiological issues.”
One way to get this information is with tiny electromechanical sensors that turn your body’s movements—such as the faint pulse you can feel when you place a hand on your chest—into electrical signals. But what happens when you receive a hug or take a nap lying on your stomach? “That increased pressure overwhelms the sensor, interrupting the flow of data, and so the sensor becomes useless for monitoring natural phenomena,” Andrew continues.
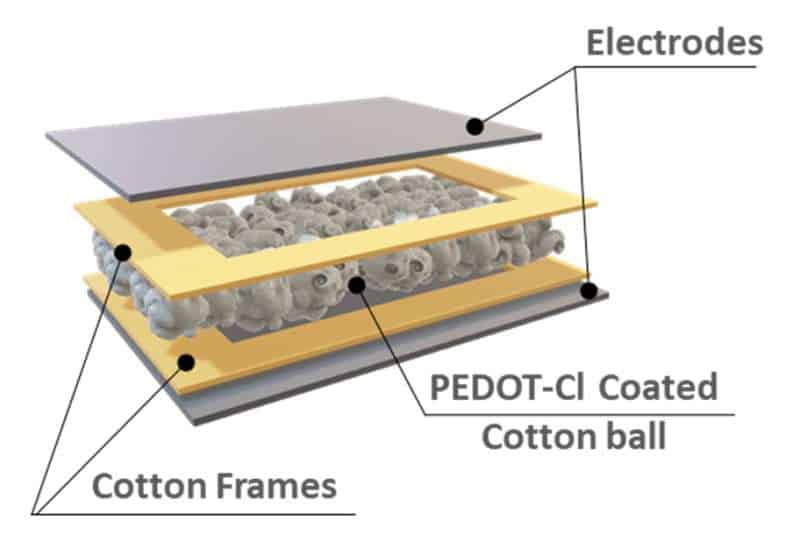
To solve this problem, the team developed a sensor that keeps working even when hugged, sat upon, leaned on or otherwise squished by everyday interactions. The secret, which was detailed in the journal Advanced Materials Technologies, lies in vapor-printing clothing fabrics with piezoionic materials such as PEDOT-Cl (p-doped poly(3,4-ethylenedioxythiophene-chloride).
With this method, even the smallest body movement, such as a heartbeat, leads to the redistribution of ions throughout the sensor. In other words, the fabric turns the mechanical motion of the body into an electrical signal, which can then be monitored.
Zohreh Homayounfar, lead author of the study and a graduate student at UMass Amherst, says that “this is the first fabric-based sensor allowing for real-time monitoring of sensitive target populations, from workers laboring in stressful industrial settings to kids and rehabilitation patients.”
Of particular advantage is that this all-fabric sensor can be worn in comfortable, loose-fitting clothing rather than embedded in tight-fitting fabrics or stuck directly onto the skin. This makes it far easier for the sensors to gather long-term data, such as heartbeats, respiration, joint movement, vocalization, step counts and grip strength—a crucial health indicator that can help clinicians track everything from bone density to depression.
Andrew and her group will next use an array of the pressure sensors under additional scenarios to determine which other types of physiological signals can be extracted, and to which level of accuracy.